
Tom says, “I have been fortunate enough to start working with the Cronulla Sharks as the U20’s physio for the
2020 Jersey Flegg season. We are currently nearing the end of the pre-season with the players being put
through their paces preparing for the season ahead.
Throughout the year I will share some of the interesting injuries which occur, how we
are managing them, and what to do if you or someone you know has similar symptoms.
For my first blog I am going to talk about lumbar stress fractures.”

Tom Mallett is the physio for the U20’s Cronulla Sharks
Lower back pain is very common and can range from anything such as a small nuisance to being
severely painful and debilitating.
Lower back pain is not as common among adolescents however it can still occur. An important
condition to look out for in this younger population with lower back pain is a stress fracture.
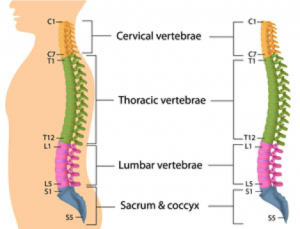
A lumbar stress fracture (or spondylolysis) is a condition affecting the bones in your lower back
(lumbar vertebrae).
More specifically it involves the posterior part of your vertebrae (parts of the posterior vertebral
arch called pars interarticularis, pedicle and lamina).
Stress fractures form from repetitive forces going through the posterior part of the spine in excess of
how much force the bone can handle. This can occur from high training loads or sports which involve
repetitive movements.

There are two different types of lumbar stress fracture. They are very important to differentiate as
management differs depending on which type has occurred.
One type is an active stress fracture which means there is current active bone stress occurring to the
part of the spine shown above. This can progress to a stress fracture and chronic defects if left
untreated.
The other type is called chronic defects. This means that a previous stress fracture has occurred and
has not fully healed, usually due to insufficient rest and rehab. This results in scar tissue filling the
fracture site instead of bone. With chronic defects there is no active bone stress.
Symptoms are very similar to other causes of lower back pain however, things that will raise
suspicion of a stress fracture include:
Symptoms will often coincide with a recent change in the amount of training/activity, but can occur
in those who are active without a recent change in activity levels.
If there is active bone stress which is occurring, management aims to reduce symptoms, allow bone
healing, return to pre-injury function and prevent recurrence. It consists of three phases:
If you are presenting with chronic defects then management involves three similar phases. However,
with chronic defects there is little chance of bone healing, so management aims to reduce pain and
restore function rather than allowing time for the bone to heal.
A brief period of unloading may be necessary to allow symptoms to settle with the length of rest
being guided by symptoms. Progression through the reloading phase and graduated return to sport
phases are also guided by symptoms.
If you or someone you know is getting symptoms similar to what has been described above then it is
important to go and see your physiotherapist as soon as possible. This condition can progress with
continued activity, so the earlier it is identified and managed the better the outcomes will be.